The aim of these operations is to relieve arm pain and or numbness and weakness affecting the arms or the legs. They are generally not designed to relieve neck pain.
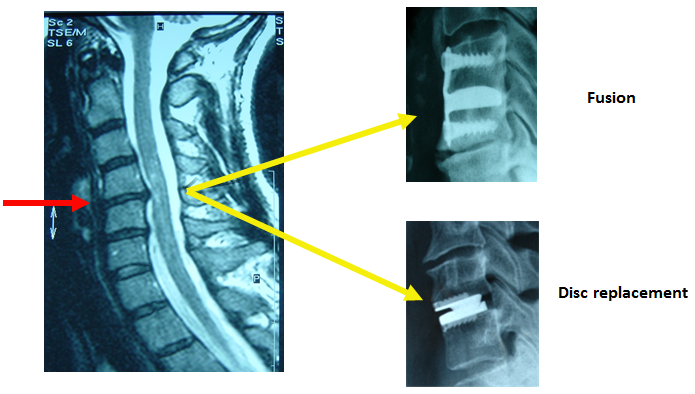
In both types of surgery the damaged disc is removed and the nerve decompressed. There is a choice as to how to reconstruct the spine after discectomy.
In total disc replacement the damaged disc is replaced with an artificial disc thus preserving motion. The design of these artificial discs has improved dramatically and is an immensely complex process which aims to restore the normal physiology.
In fusion the damaged disc is replaced with a bony bridge between the vertebrae. This stabilises the two bones/vertebrae. Again, the devices used to achieve fusion are complex and represent a major advance on methods available only a few years ago. They usually involve plates, cages, screws and bone graft which may be artificial or harvested from you.
Fusing a disc inevitably transfers work to the adjacent discs. So, unless there is a good reason to fuse the spine, the usual course is a disc replacement as this offers to restore and or preserve movement at the affected level.
Disc replacement is therefore now more common than fusion after disc removal though the evidence that it is actually better is not as tight as you might think. Both operations are good. Your big decision is whether to have surgery or not. If you have spent more time thinking about replacement vs fusion your mind has been focused on the wrong issue - though this is an important decision too.
Fusion is needed if there is significant instability at the operated level – spondylolisthesis or if there is a fracture as well as a prolapse.
Fusion is also used if the disc space is already very narrow when the movement has already been lost. If the facet joints are also worn and painful then disc replacement can make this worse. Finally, if there are a lot of osteophytes then these have to be drilled away. As a result of this bone work, the two vertebrae can fuse around the replacement – this happens more often with some discs than others and may occur as many as one in ten times.
Disc replacement is not a guarantee of no more trouble nor does it prevent all disease in the adjacent levels. You wore out the first disc without having had a fusion so you may also wear out another. That said, our philosophy is to preserve and restore function where possible.
Is there good evidence to prove disc replacement is better? Not in the form of randomised trials. Such trials are difficult to do, they have been flawed and to some degree inconclusive. In our view, this reflects the difficulty of doing this kind of study. For most patients, a logical choice can be made and where there is doubt we would opt for disc replacement – you can fuse after if it does not work but you cannot reverse a fusion.
The Operation: Cervical Discectomy
Once you are anaesthetised, you are placed face up on the operating table. A horizontal, gently curved incision, approximately 3 cm long, is made just to the right of the Adam’s apple usually within an existing skin crease.
We use an X-ray machine (Image Intensifier) to help us locate the correct position. Local anaesthetic is used to numb the nerves in this area and so lighten the anaesthetic needed. The muscles on the side of the neck are then parted and the front of the spine identified and exposed. The correct level is then again confirmed with an X-ray. Special retractors are used to hold the soft tissues safely aside – these include the larynx (wind pipe), the oesophagus (swallowing tube), carotid artery and jugular vein. Another special distractor instrument is then used to hold the vertebral bones slightly apart so as to create space to work in. It spans the bones and discs to be operated on/removed. Everything up to this point is referred to as “access”.


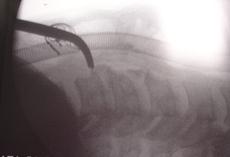
Access is gained via a small incision on the front of the neck and is guided by X-Ray
The operating microscope is then brought in and the surgeon works thereafter looking through this scope – it brings superb illumination as well as magnification to allow precise operating. Now the main part of the operation begins.
Gradually, the back of the disc and any osteophytes are cleared and the central canal is exposed thus gradually relieving the pressure on the spinal cord. This surgical part of the procedure is termed central canal decompression and the operation has slowed to a snail’s pace at this point as the spinal cord is immediately below. A specifically designed high speed air drill is used to carefully drill away any compressing bone.
The nerves exiting the spine on either side are now cleared of any disc prolapse or osteophytes. This element of the operation is termed nerve root decompression. The removal of the disc prolapse itself is termed a discectomy.
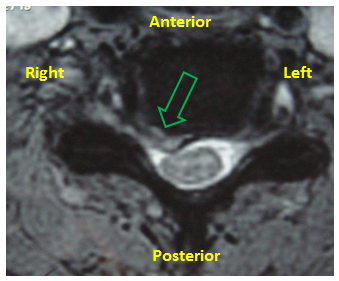
A degenerate disc is seen prolapsed and compressing the exit of the right nerve root as well as distorting the spinal cord. The nerve roots are compressed on both sides more laterally by bulging disc material.
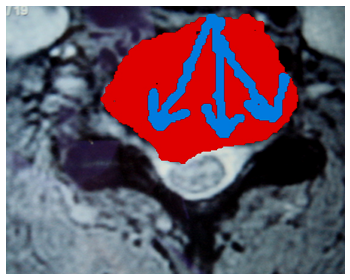
Here the red area and blue arrows indicate the area that is cleared in discectomy and nerve root decompression.
Reconstruction
Following a discectomy, there are two different methods for cervical spine reconstruction: disc replacement or a spinal fusion.
Prior to the surgery we will have discussed which is the best method of reconstruction for you. Disc replacement or fusion: which is best for me?
Once the decompresion is complete and the damaged disc has been cleared the ends of the exposed bones above and below are meticulously cleared of all fragments of disc and soft tissue so as to expose healthy bone. This is crucial if the plates of the artificial disc are to bond to the bone. Unlike in fusion reconstruction, no bone graft is needed for this operation and so no extra incisions are needed to harvest it.
Before the surgery we will also have discussed with you the range of artificial discs available and will recommend the one we feel appropriate for you. We feel the choice is crucial.
Disc Replacement
Once you have had your offending disc removed a disc replacement procedure can be performed as the cervical spine reconstruction.
Closure
After the reconstruction is complete, the wound will then be stitched in layers using internal absorbable stitches. Often the final stitch runs under the skin and has to be removed some five days later.
Informed consent
Before you have a procedure of any kind, however trivial you may feel it to be, you must be fully aware of the possible and likely consequences. You have to sign a consent form in which you state that you are fully aware. We will go over this with you in your consultation. Do not sign the consent form for a procedure with us unless you feel fully informed of its aims and risks, as well as the alternatives.
Please make sure you are fully content with everything set out in our Informed Consent for Treatments: Operations and Injections.
What alternative procedures are there?
Much of this will have been discussed in our consultations. Essentially, an operation is always the last resort. Instead, you could try injections or further conservative treatment (physiotherapy, osteopathy, chiropractic, acupuncture, tablets and time). Obviously, we will usually have formed the view that these are unlikely to bring you to comfort any time soon before recommending surgery. For the majority, it is pain that drives the surgery. In these circumstances, you have to feel that the degree of pain warrants the risk and effort involved in putting yourself through the operation.
What are the Risks?
No procedure is without risk, though these are routine operations which rarely cause harm. If you would like to read an extended list regarding the risks of this particular type of surgery. Please click here for full details.
No procedure is without risk, though these are routine operations which rarely cause harm.
Chest infection and blood clots in the deep veins of the legs – these complications can result after any operation and indeed after any long period spent in bed. We can reduce the incidence of these by giving you injections to thin the blood, supportive stockings and compression pumps on the legs worn while in bed.
Risk to life and limb – Any anaesthetic and any operation may kill you. Any spinal surgery may paralyse you which in the instance of a cervical operation could mean loss of all arm, leg, bowel, bladder and sexual function. These disasters are extraordinarily rare. People do get run over by buses but it is exceptionally rare.
Swallowing – Problems with swallowing such that food feels difficult to get down or blocks can arise temporarily after the surgery but seldom persists for more than a few days. Likewise, the hoarseness of voice.
Nerve root injury – the nerve root is often handled during the procedure and microsurgical technique is used to reduce any damage. However, the risk of an individual nerve being permanently lost is around 1%.
Failure of an operation to achieve its intended goal is always possible. It is not uncommon for a degree of pre-existing weakness and numbness to persist.
The longer they have been present, the more likely this is. However, most patients experience an improvement, if not a complete resolution of their symptoms.
Recurrence of symptoms may occur. Post-operative physiotherapy plays an important role here. Scarring around nerve roots that are hypersensitive from previous surgery or a recurrence of the original disc prolapse can occur.
Operations simply tackle current troubles and offer no protection against future problems but post-operative physiotherapy can.
Deterioration – this is a possibility. Operations can make you worse, can do you harm or may leave you with new problems to cope with. This is rare and affects fewer than 1% of patients.
Wound infection can occur with any operation. In the spine, this is rare as there is so much muscle covering it. Muscle fights infection well. However, if an infection does set in, the effects can be very serious.
When can I go home?
Most people go home on or around the third post-operative day.
Post-operative neck care
Before you go home after your operation, we will have discussed some details of how to care for your neck in the weeks that follow. Please click here for a general summary.
Physiotherapy
If you develop pain on doing your specific instructed exercises, you should stop them. In the first few weeks, all that can occur is the simple healing process. Physiotherapy maintains your mobility during this time but should not be allowed to interfere with the healing process. Therefore, if it hurts you should stop. Physiotherapy begins in earnest around the fourth week when the wound and neck will be stable enough to allow real progress to be made.
Exercise
The aim here is to do small amounts but often. Problems arise when patients do a little too much a little too often. For most of the first week, you will either be in hospital or should be pottering about inside your home. For the second week, the amount of activity undertaken should essentially be unchanged. You should not be doing housework or looking after others. You may go out for short walks. From the second week onwards, light exercise may be undertaken. You may go on very short car journeys (10-15 minutes) and go out for longer walks. Prolonged outings and lengthy trips to the office will be bad for you.
Sitting
You are better to sit upright and not to have the neck bent by cushions. When lying on your back in bed, do not use too many pillows. Be careful about time spent sitting at a computer as this tends to stiffen the neck.
Baths and showers
You should in the early days avoid baths as any waterproof dressing is unlikely to keep out all water if submerged. Showers or and assisted standing baths are better. Please do not fall over.
Sex
If it hurts, don’t. If you think it will hurt, don’t – until of course you think it won’t and it doesn’t.
Wound care
You should not get the wound wet until the day after the sutures have been removed. It is perfectly reasonable to have a shower, providing the wound is covered with a waterproof dressing. The ward may provide you with this before you leave. It is best to cover the wound in a waterproof dressing for showers but this should be replaced by a dressing which breathes – ask our spinal nurse which ones you need.
Removal of stitches
The stitches, of which ever type, should be removed at or shortly after the fifth day from the neck but not until the tenth day from the hip. Most often a nurse linked to your GP or the district nursing service do this. You need to have agreed an arrangement for this to be done before you leave hospital – our ward nurses will liaise with your GP, district nurse or your local hospital as appropriate. You will also be given a ‘clip remover’ for you to give the nurse who will be doing the removal.
Bending, lifting, carrying
In the first few weeks, you should not be doing this. The physiotherapy, which will usually begin about the fourth to sixth week, will teach you how to bend correctly and how best to lift. It should certainly be something that you keep to a minimum in the first months.
Driving
In the first few weeks, you should be driven i.e. you should not drive the car yourself. In the weeks that follow, you should limit journeys to short periods. In general, it is best to have the car seat set as high and as upright as possible. Unless you can look over your shoulder, you are not considered safe to drive. If in doubt, do not drive until we give the all clear.
Sports
You should not do this until we have reviewed your progress. If should be deferred until you have completed the fitness programme that only begins with the physiotherapy at the fourth to sixth week and is likely to take a further four to six weeks at least.
Our general philosophy
The aim is for you to avoid things which aggravate your pain. Once recurrence of neck and arm pain has occurred, it is much more difficult to go away. It is much simpler to avoid it in the first place. It is not so much what you do but how often you do it.
*If you feel you are developing unexpected troublesome or worrying symptoms, do not hesitate to call The Spine Surgery London or the ward staff, who will be able to guide you. Please go to Contact Us page for suitable contact numbers.
When will I next see you after my operation?
Our usual routine is to see patients three to four weeks after discharge and it is at this point that we can start the physiotherapy. Often there is a need for follow-up X-rays so it is useful to have the old ones for comparison, so please bring these with you. We usually then see you after another six weeks and then after a further three months.
When can I go back to work?
This may reasonably be anytime between four and twelve weeks post surgery. Please click here for a extended information.
This might seem like a ridiculously wide window and certainly we will advise you more precisely. In fact, some patients are back at work inside two weeks and others still off at four months. Whatever the work, a gradual return is best. Days spent working from home may help. However, done in a graduated way, the return to work is a very positive part of your rehabilitation. It needs to be in your control and with the encouragement of your employer. If they can put up with you being part-time and unreliable, they will see you sooner. Discuss the advice we give you and make a plan with your employer.
What do I do in the event of problems?
If, once you get home problems arise, help is available from a number of sources. Firstly, if it is during working hours, you may ring The Spine Surgery London. If it is out of hours, our voicemail will tell you what to do in the event of an emergency. Secondly, you may ring the hospital and ask to speak to our Spinal Nurse Specialist. In her absence, you should ask to speak to the hospital’s Duty Manager or to the ward staff (please go to Contact Us page for more information).
You may of course contact your general practitioner or any emergency service, should you so wish or if the other avenues fail.
We do not provide a 24 hour emergency service but can respond on most occasions.